Alzheimer’s disease and dementia represent one of the key global challenges affecting our society impacting over 55 million people worldwide and 13,625 individuals in Northern Ireland.
Scientists from Ulster University are working on world-leading research into better understanding dementia and Alzheimer’s disease with the aim of enhancing timely diagnosis for patients and novel treatments for Alzheimer’s disease.
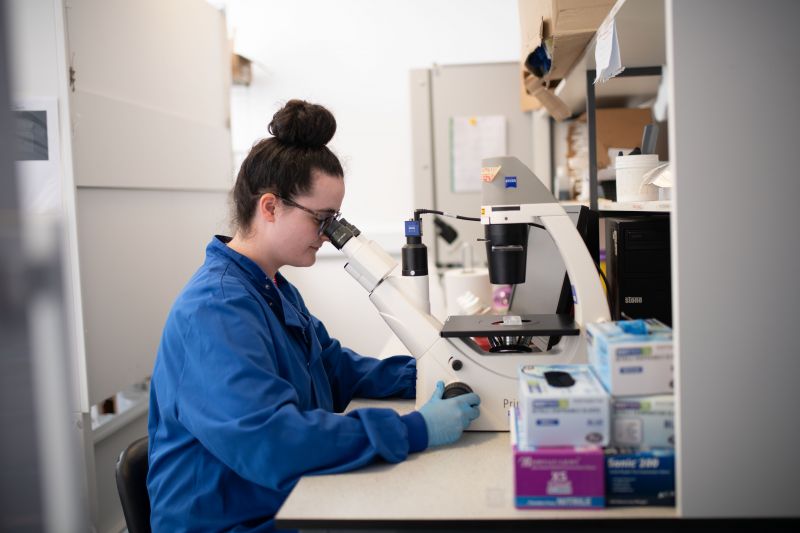
Research is underway at the Personalised Medicine Centre, located in the School of Medicine at the University's Derry~Londonderry campus and Altnagelvin Hospital, by a team of local researchers involving dementia and Alzheimer’s patients from the local area.
The challenges
So much about dementia is still unknown and there is a pressing need to improve and shorten the diagnostic process and for effective and affordable therapeutics. Diagnosis of dementia takes a long time and is primarily based on the clinical judgement after assessment of neuropsychological test scores and imaging of the brain. It is still the case that a definitive (firm/definite) diagnosis cannot be confirmed until a post-mortem has taken place.
Diagnosing different types of dementia is difficult, and misdiagnosis affects the quality of care and appropriate access to services.
Researchers are aiming to answer the unknown questions surrounding dementia by investigating different causes of dementia and also different subgroups of Alzheimer’s disease. The aim is to reduce diagnostic delays for patients, and identify safe, affordable, drugs for the treatment of Alzheimer's disease.
Finding solutions through research
One approach from the field of personalised medicine that the researchers are exploring is the analysis of biomarkers from blood samples in order to differentiate between dementia subtypes and Alzheimer’s disease. Blood-based diagnostic tests would significantly reduce the time taken to diagnose and permit timely access to treatment, so has the potential to greatly impact patient outcomes. This is extremely important if drugs to treat the underlying cause of Alzheimer’s disease become widely available.
Evidence suggests that an early diagnosis provides dementia patients with the chance to live independently in their own home for longer, avoiding early or unnecessary admission to a care home or hospital, enhancing their quality of life and providing substantial savings on long-term care costs. Drug and non-drug treatments can be more effective the earlier someone is diagnosed.
Ulster University’s research focusing on early detection, more accurate and faster Dementia diagnosis willfurther compliment drug developments, most recently the donanemab drug which has been hailed as a turning point against the disease, slowing clinical decline by up to 35%. However optimal results for patients using this drug rely on an early and accurate diagnosis which is currently detected using a limited supply of PET scanners in the UK, meaning that only 2% of the population will be diagnosed early enough for this new drug to have a real impact.
Senior Lecturer of Personalised Medicine, Dr Paula McClean, from Ulster University’s School of Medicine explained the significance of this research study;
“At the Personalised Medicine Centre we are focusing on evaluating blood-based biomarkers, which may be used to diagnose disease. The overall aim is to enable differential dementia diagnosis that can help us to identify different types of dementia and subtypes of Alzheimer’s disease, so that patients can receive an accurate and timely diagnosis and that more targeted and effective therapies can be identified.”
“Another area of research at the Personalised Medicine Centre is drug repurposing studies, in which researchers are looking at drug treatments that exist for other conditions to establish if they may be effective in the treatment of Alzheimer’s disease. The hope is that they may identify effective – and, importantly, – affordable treatments for Alzheimer’s which would be available sooner rather than later as approved drugs will have undergone significant safety testing already."
Paula explains: “Alzheimer’s disease dementia is a life-limiting illness which varies considerably from person to person. Some individuals experience a fast decline in cognitive function whilst others decline much more slowly. We are linking all health-related history to determine what factors influence disease progression and aim to evaluate whether this may be predicted by biomarkers. We are very grateful to members of the public who are actively participating within our clinical studies. Research offers hope to many families affected by dementia and, without their participation, new medical developments would not be possible.
“Existing treatments which treat the symptoms of Alzheimer’s are widely available, however, they do not treat the disease itself and are, unfortunately, not effective for all patients. In the last year, two new drugs have been approved for use in the USA, however approvals have not yet been granted in Europe and the UK.
“Whilst this seems like a promising step forward for those affected by Alzheimer’s disease and their families, these drugs are expensive and unlikely to be accessible to the worldwide population who urgently need them. The majority of those with dementia are from low- and middle-income countries therefore it is imperative that new drugs must be affordable – this a priority for PMC researchers.
“Additionally, there are some safety concerns which mean that patients taking these drugs have to be closely monitored through MRI scans which are associated with additional clinical time and access to MRI infrastructure that is not widely available to the populations in many low- and middle- income countries.
“This means that there is a critical unmet need for affordable, safe, disease modifying drugs for the treatment of Alzheimer’ disease. Those working in the PMC are exploring a number of disease modifying drugs that target the underlying causes of Alzheimer’s disease. Researchers are excited by the potential of one of the drug candidates that has shown significant promise in a preclinical model of Alzheimer’s disease. With further research, they are hoping it would represent a safe, effective and affordable therapeutic strategy for all of those affected by Alzheimer’s disease.”
The study involves collaboration with Queen’s University, local clinicians in the Western Health and Social Care Trust, Alzheimer’s disease charities and the Learmont Dementia Friendly Hub.
Clinical research undertaken within the PMC was supported by research grants from the European Union Regional Development Fund (ERDF) EU Sustainable Competitiveness Programme for N. Ireland; Northern Ireland Public Health Agency (HSC R&D) & Ulster University and the European Union’s INTERREG VA Programme, managed by the Special EU Programmes Body (SEUPB).
Drug development research has been part-funded by INVEST NI’s proof of concept programme, contributing £140,000 investment. Additional investment in dementia research is urgently needed to accelerate the pace at which discoveries can benefit patients. The Personalised Medicine is actively seeking investors/donations to advance this work at pace.
Leading healthcare research from Derry-Londonderry
These are just some of the multiple research projects designed to improve healthcare which are currently ongoing at the Personalised Medicine Centre, which this year marks its 10th anniversary of being at the forefront of innovation in personalised and precision medicine.
Studies led by the team include research into multiple long-term conditions such as cardiovascular disease, diabetes, blood cancers, vision, neurodegenerative disorders and arthritis. The Centre represents a £25million funding investment and, since its establishment in 2013, it has been leading data-driven research, innovation and education designed to improve healthcare provision and patient outcomes. Its expert team of almost 60 Ulster University staff and PhD researchers and over 20 Western Trust clinical leads, conducts research studies for future implementation in clinical settings that tailor medical decisions and interventions to an individual.
Personalised medicine moves away from a one-size-fits-all approach to better manage patients’ health and targets therapies to achieve better outcomes in the management of the patient’s disease. It relies not only on the reading of human genomes but requires the collection of large amounts of personal, clinical and lifestyle data supported by underpinning technologies such as consumer apps and wearable technologies.
Integrated into the University’s School of Medicine, the Personalised Medicine Centre contributes to the delivery of the School’s ambitious vision, teaching both undergraduate and postgraduate students in personalised medicine, as well as on the MBBS, Physician Associates and University's Biomedical Sciences degree programmes.